In fall of 2012, I was in my senior year at NYU. It had been a year since major depressive disorder and generalized anxiety disorder nearly shut down my body, mostly through merciless sleep deprivation.
My psychosomatic symptoms were still a daily gauntlet. For me, a “good” night of sleep was five hours with two or three interruptions. Unintentional all-nighters remained a regular part of my schedule, albeit less frequent than my junior year. Falling asleep took at least two hours of meditation and slowly rolling around my mattress-topped foldable futon. A few times a week, random parts of my body ached acutely, sometimes causing me to wince noticeably in the middle of class.
To sleep and prevent myself from experiencing withdrawal, I took 60 milligrams of Duloxetine — also known as Cymbalta — every morning. My psychiatrist was an NYU-based nurse practitioner named Janet. She was kind to me. Although her job was only to manage my medication and ask me about symptoms, she seemed to care about my life goals and relationships.
It was my second year of therapy, and I was on my third therapist, Leslie. He was not part of the NYU system like my last therapist, but his office was near “campus” (NYU doesn’t have an official closed campus, but there are a cluster of buildings near Washington Square Park). I liked Leslie. The therapy seemed to be helping me.
Fall, 2012 was one of the only semesters when I didn’t have a part-time job. Because I had worked nearly every summer and semester, my parents and I agreed I should take it a little easier my senior year.
Instead of relaxing, I regretted the decision and felt guilty. My private college education had been a financial strain on my parents, who were doing fine but weren’t wealthy by any means. Their health insurance supported my therapy and medication. They were in debt, and soon I would be, too.
I had an existential anxiety of being a burden, a net negative; to my parents, to my classmates, to my professors, to my roommate who had already endured a year of proximity to my pain, to the world.
I told myself my life needed to become a net positive. If I couldn’t achieve that outcome, it would be better if I hadn’t existed at all.
Simultaneously, I judged and resented those who were receiving more support than me, especially those who seemed to be squandering their resources. My parents had said I could take a semester off to deal with my illnesses, but I didn’t believe them. Other kids could do that, not me. If I had taken time off, I would’ve beaten up on myself and felt weak.
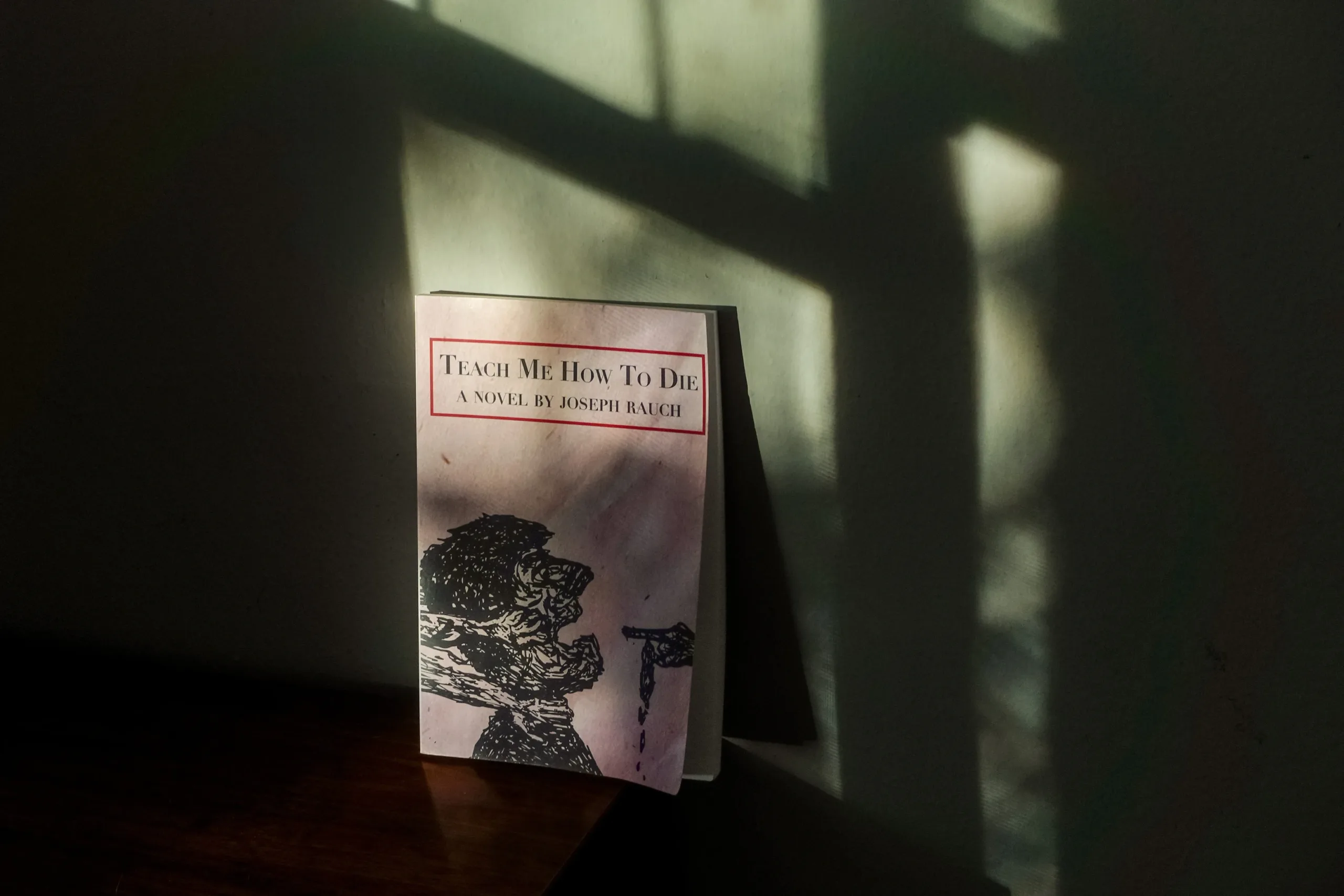
As part of my psychology major, I was taking a class on abnormal psychology. The professor was David Wolitzky. During his lecture on the history of asylums, the core idea for “The Last of the Mentally Ill” sprung into my mind, and I scribbled a separate page of notes next to my class notes.
It all started with Chester and Claire. Chester was the embodiment of my anxiety and insecurity. I wanted him to triumph. Claire was the embodiment of my self-hatred and judgment toward others. For me to resolve my internal conflict, Chester had to defeat Claire, to show she was wrong.
To understand the rest of what inspired “The Last of the Mentally Ill,” you’ll have to read the afterword at the end of the book. If you have more questions, you can get the answers by joining our Patreon community starting at only $1 a month.